Table of Contents
What can BCBAs do to prevent burnout?
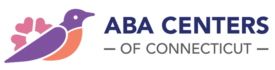
Burnout in BCBAs has become an increasingly discussed topic across the field of applied behavior analysis, reflecting the evolving demands placed on today’s clinicians rather than a single underlying cause.
Burnout in BCBAs is not limited to a single setting, population, or career stage. It often develops gradually, shaped by a combination of clinical responsibility, professional expectations, and the realities of balancing high-quality care with long-term sustainability.
For many clinicians, burnout does not present as a dramatic breaking point. Instead, it emerges as ongoing fatigue, reduced emotional bandwidth, or a growing sense that the work requires more energy than it once did.
Understanding how burnout develops and how to prevent it requires looking at both professional skill-building and workplace structure together. So, what can BCBAs do to prevent burnout? At a high level, avoiding burnout involves aligning caseloads with clinical capacity, strengthening boundary-setting and time management skills, using supervision and peer support effectively, and working within environments that value balance and professional growth.
This blog by ABA Centers of Connecticut explores burnout in BCBAs through a practical, evidence-informed lens.
Understanding the Scope of Burnout in BCBAs
A Board Certified Behavior Analyst (BCBA) operates in a role that blends clinical decision-making, ethical responsibility, supervision, parent training, and payer compliance. According to the BACB, BCBAs are graduate-level professionals responsible for designing, overseeing, and evaluating behavior-analytic interventions, often while supervising multiple team members across cases and settings.

This broad scope helps explain why burnout in BCBAs can be an aspect of the role’s complexity rather than personal resilience alone. ABA professionals require clinical judgment, emotional engagement, and sustained attention across multiple contexts, often within tight timelines. Over time, this level of cognitive and emotional demand can contribute to burnout if not intentionally managed.
Research across healthcare and behavioral health consistently links burnout to prolonged exposure to high job demands without adequate recovery or support. In ABA, these demands coexist with meaningful, purpose-driven work, which can sometimes delay recognition of burnout until symptoms are well established.

Rather than reflecting a failure of individuals or organizations, burnout in BCBAs is most accurately described as a multifactorial professional challenge.
It develops at the intersection of workload, role expectations, career stage, personal coping strategies, and workplace resources.
A study examining burnout and engagement among behavior analysts found that emotional exhaustion and depersonalization were common, particularly when clinicians experienced limited flexibility and sustained workload pressure. Notably, the findings highlight that both individual strategies and organizational practices influence burnout risk.
This balanced view matters. When burnout is framed solely as an individual issue, solutions focus narrowly on self-care. When it is framed solely as an organizational issue, we minimize clinician agency. The evidence suggests burnout prevention is most effective when the parts share responsibility across professional development and workplace design.
Support for Work-Life Balance for BCBAs
While work-life balance can sound abstract, for many BCBAs it translates into efficient concerns: time allocation, emotional recovery, and the ability to disengage from work demands outside of scheduled hours.
The BCBA State of the Profession Survey indicates that administrative responsibilities and competing demands are frequently cited contributors to burnout. These findings reflect the growing complexity of the BCBA role rather than dissatisfaction with clinical work itself.
Why Work-Life Balance for BCBAs is a Clinical Competency
Work-life balance for BCBAs is a professional competency that supports ethical decision-making and clinical consistency.
Sustained fatigue and cognitive overload can affect data interpretation, supervision quality, and responsiveness to clinical change. Maintaining balance helps preserve the attention and judgment required for effective practice.
Recognizing Early Indicators of Burnout in BCBAs
Burnout in BCBAs often develops through gradual changes in emotional, cognitive, and behavioral functioning. Common early indicators include:
- Reduced emotional engagement with cases or teams
- Difficulty concentrating during assessments or program reviews
- Heightened frustration around scheduling or documentation
- A persistent sense of inefficacy despite strong effort
- Decreased participation in professional collaboration

These indicators are consistent with broader burnout research in healthcare professions. Identifying these patterns early allows clinicians and organizations to respond proactively rather than reactively.
Evidence-Based Strategies to Reduce Burnout in BCBAs
Preventing burnout in BCBAs requires practical strategies that address both daily workflow and long-term professional development.
- Job Crafting and Role Alignment: Job crafting, making intentional adjustments to how work is structured, has been associated with improved engagement and well-being among behavior analysts. For BCBAs, this may involve refining documentation systems, clarifying role boundaries, or aligning caseloads with areas of clinical strength.
- Supervision and Professional Connection: Supervision and peer consultation function as critical professional resources. Studies using job demands–resources frameworks emphasize their role in buffering stress and supporting ethical practice. Regular consultation helps normalize challenges and reduces the isolation that can contribute to BCBA burnout.
- Emotional Skill Development: Emerging research suggests that emotional intelligence may influence how workplace stress relates to burnout in behavior analysts. These findings support the value of developing emotional awareness and stress-regulation skills alongside technical competence.
Burnout in BCBAs and Professional Retention
Burnout not only affects individual clinicians but also affects the sustainability of the field. Research by Behavior Analysis in Practice examining behavior-analytic practitioners’ intention to leave positions or the profession found that burnout-related variables were strongly associated with turnover considerations.
From a field-wide perspective, addressing burnout supports continuity of care, professional development, and long-term workforce stability.
Supporting Sustainable Practice Moving Forward
The industry should approach burnout in BCBAs as a shared professional challenge that evolves alongside the field itself.
When clinicians have access to supportive supervision, manageable workloads, and opportunities for growth, they can sustain high-quality care over time.
At ABA Centers of Connecticut, we are continually working to foster a practice environment designed with sustainability in mind. We provide intentionally low caseloads to support balance, offering competitive career benefits, and investing in professional growth through our in-house training academy.
If you are a BCBA or on the path to becoming one and are looking for a practice environment that prioritizes balance, ethical care, and professional support, we invite you to explore our open positions on our website or contact us directly at (844) 395-0448 to learn more.
Taking that step is entirely optional, but for many clinicians, it’s the beginning of a more sustainable way to practice.